Selective Laser Trabeculoplasty
What Is SLT?
Glaucoma management can consist of:
- Medications (eye drops or tablets)
- Laser
- Surgery
- Any of the above combinations
Selective Laser Trabeculoplasty (SLT) is simply another method of managing intraocular pressure, but by using Laser.
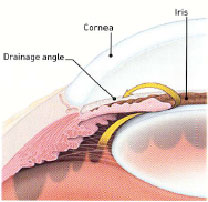
The critical element determining whether you are suitable for SLT is whether your trabecular meshwork (internal drains of the eye found at the drainage angle) can be adequately seen by the doctor using specialised lenses.
The trabecular meshwork is a sieve-like structure found inside eyeball, at the junction between the peripheral cornea (clear glassy window at the front of the eye) and the iris (coloured part of the eye). This structure drains the aqueous fluid from within the eye. Note: Aqueous fluid is very different from tears that are produced to coat and wash the outside surface of the eye.
In glaucoma, the trabecular meshwork doesn’t drain efficiently.
How does SLT work?
SLT is a new generation of “cold” lasers, because it does not hurt or destroy the underlying trabecular meshwork where the laser is applied.
The SLT laser beam is instead selectively absorbed by pigmented cells of the trabecular meshwork, sparing the surrounding non-pigmented structures of the trabecular meshwork from damage. It excites (upregulates) the body’s own cleaning cells (macrophages) to remove debris / substances that are blocking the trabecular meshwork – somewhat like removing the food scraps from your kitchen sink sieve to allow better drainage of fluid from the eye. This is the mechanism of how SLT lowers your intraocular pressure.
Is SLT Successful In All Cases?
Approximately 70% of SLT is successful after only one treatment. Of approximately 30% of patients that require a second treatment of SLT, 70% of these patients will respond. This means that after 2 treatments of SLT, almost 85%-90% of people are expected to have a good response.
Of course, every eye is different and your treatment will need to be tailored individually to your needs by your treating doctor. Unfortunately, some patients will not get any pressure reduction despite successful application of laser.
Post Laser Management
You must continue ALL your current anti-glaucoma eye drops as usual after the SLT treatment until your next appointment. At that next clinic review, your medication regime will be reviewed and optimised.
Some patients notice a dull headache or a bruised sensation after the laser procedure. This is often associated with the preparatory eye drops (called pilocarpine) used before the laser surgery.
Pilocarpine has the action of (1) opening the drainage angle for safe laser application and (2) lowering the intraocular pressure to prevent the post-laser pressure rise. It is acceptable to take additional paracetamol / aspirin as directed by your treating doctor.
If the pain does not significantly resolve following the paracetamol / aspirin, contact your eye doctor for further advice.
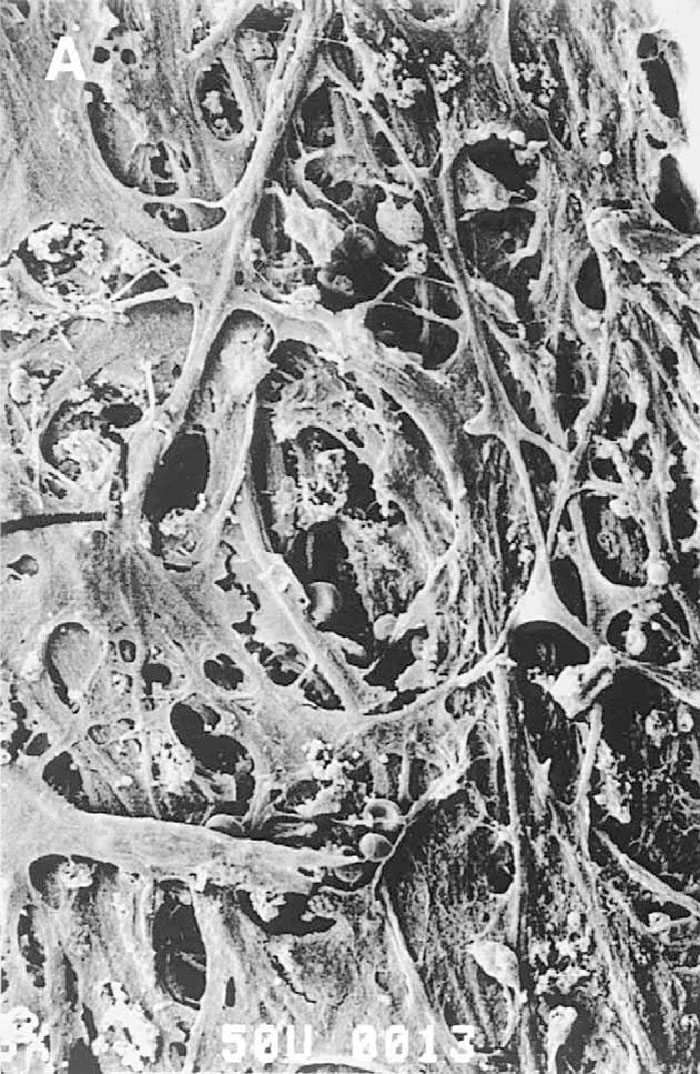
Figure: Electron microscopy of trabecular meshwork. Notice the sieve-like nature of this structure
Frequently Asked Questions
How is it performed?
SLT is performed as an office laser procedure. This means that we can perform this under local anaesthetic drops, with no need for needles, injections or eye patching. The entire process takes approximately 1- 2 hours as we need to prepare the eye with drops before the laser procedure, and then recheck the eye after it is all completed. The laser procedure itself usually takes several minutes only.
Are there any complications?
All procedures have the potential for complications. SLT has been performed around the world for millions of people with open angle glaucoma for many years with good success, and minimal risk of complications.
One potential complication of SLT is to suffer a significant rise in eye pressure. This is usually prevented with the use of eye drops before the laser surgery. If there is a rise in eye pressure, it is often temporary and manageable with eye drops or tablets. There is a small risk of <1:500 for the need to proceed to surgery if the pressure remains constantly high and not controlled with medications.
Booking an appointment
You will require a valid referral to claim your consultation fee and associated investigations from Medicare. Referrals from your GP or Optometrist are valid for 12 months, however specialist referrals are only valid for 3 months.
If you require any specific information regarding your eye problem, for example cataract or glaucoma consultations, we ask you kindly ring your desired practice for fees and further information.
Urgent Appointments
If you have any urgent query or problem, we request that patients or referrers ring the practice directly and speak with a staff member. We will always do our best to accommodate for urgent referrals, or direct you in the best possible manner.
How to reach us?
Dr Brian Chua's primary consulting locations are St Vincent's Clinic and Gordon Eye Surgery.
Please ring us if you require any further information or wish to book an appointment.
St Vincent's Clinic Ophthalmology
Level 10 Suite 1006
438 Victoria Street
Darlinghurst NSW 2010
Ph: 02 8382 6030
Fax: 02 8382 6031
Email: eyedocs1006@stvincents.com.au
Gordon Eye Surgery
2/741 Pacific Highway
Gordon NSW 2072
Ph: 02 9418 1488
Fax: 02 9418 4392
Email: info@gordoneye.com.au
St Vincent's Clinic Ophthalmology
Address: Level 10 Suite 1006
438 Victoria Street Darlinghurst NSW 2010
Tel: 8382 6030
Gordon Eye Surgery
Address: 2/741 Pacific Highway Gordon NSW 2072
Tel: 9418 1488
Lane Cove Eye Surgery
Address: 304/71 Longueville Rd, Lane Cove NSW 2066
Tel: 8377 7600