Glaucoma
Diagnosis
Glaucoma can only be diagnosed on the basis of multiple sources of information, that includes a comprehensive history, assessment of risk factors, and a full ocular examination including the structural and functional characteristics of the drainage angle and optic nerve head. Intraocular pressure measurements are only one small component of this process, and should not be relied on for a diagnosis. Sometimes before a diagnosis of glaucoma can be confirmed, you may require repeated evaluation of the optic nerve structure and function to look for evidence of change or progression over time.
Risk Factors Of POAG
There are several risk factors for primary open angle glaucoma. These include:
- Age
- Family history
- Intraocular pressure
- Ethnic origin
- Refractive error
- Central corneal thickness
- Diabetes
- Systemic hypertension (high blood pressure)
- Long term steroid users
- Migraine and peripheral vasospasm
- Previous eye trauma
What Is Glaucoma?
Glaucoma refers to a group of diseases that affect the optic nerve head, the structure of the optic nerve that connects to our eyes. The cause of this damage is varied and there is a worldwide consensus among ophthalmologists that an elevated intraocular (inside the eye) pressure is just one facet of this complex condition.
The optic nerve, made up of millions of nerve fibres—like an electrical cable, is critical for the transmission of information from the eye to the visual centres of the brain. In glaucoma, because damage is confined to the optic nerve head, characteristic visual field defects or “blind spots” can result. Glaucoma is often referred to as the ‘sneak thief of sight’ because early glaucomatous visual field changes can only be detected with formal visual field testing.
Worldwide, glaucoma is the leading cause of irreversible blindness. It affects 1 in 10 Australian’s aged over 80 years old. Up to 50% of people with glaucoma are unaware of their disease as it remains undiagnosed. Early detection and treatment by your eye care practitioner is the key to preventing optic nerve damage and blindness.
Treatment
Current glaucoma management is based on the triad of medications, laser surgery, incisional surgery, or any combination of the three.
Medications help by either reducing the production and inflow of aqueous fluid into the eye, or by increasing the outflow pathways to allow aqueous fluid to drain more effectively from the eye. The critical factor with medications is that it requires cooperation from patients. Remember, drops can only work if you use them.
Laser surgery may be performed in some cases of glaucoma. Different lasers are used to treat open and closed angle glaucoma. Laser can be applied to the iris or the trabecular meshwork to allow aqueous fluid to flow more effectively within the eye as well as drain more efficiently from the eye.
Incisional surgery (trabeculectomy or glaucoma drainage devices) may sometimes be required if the disease cannot be controlled using medications or laser, or the patient is intolerant of the above strategies. The requirement for incisional surgery becomes more urgent the more advanced your glaucoma becomes. The surgery creates an alternate pathway for aqueous fluid to exit into the space just under the whites of the eye, beneath the upper eyelid. Aqueous fluid will then be absorbed by the fine blood vessels that are naturally found on the whites of the eye.
Types Of Glaucoma
Glaucoma is often categorised in terms of whether the angle is open or closed. The angle describes the space inside the eye where the peripheral iris (coloured part of the eye) meets the peripheral cornea (clear window) on the internal surface at the front of the eye. The importance of the angle is that this is where the trabecular meshwork is found. The trabecular meshwork is a ring of tissue which is the main outflow drainage pathway of aqueous fluid from the eye.
Aqueous fluid is constantly produced within the eye, and circulates to provide nutrients and remove wastes to sustain the delicate internal structures of the eye. Additionally, it maintains a constant pressure within the eye to keep the eyeball inflated. It should be noted that aqueous fluid is entirely different to tears, which are found and produced on the outside surface of the eye to lubricate, provide nutrients and remove waste and debris from the outside surface of the eye. To maintain a stable pressure within the eye, the rate of aqueous inflow must equal the rate of aqueous outflow. When this becomes unbalanced, and the outflow of aqueous fluid does not keep up with its inflow, the pressure within the eye (intraocular pressure) rises.
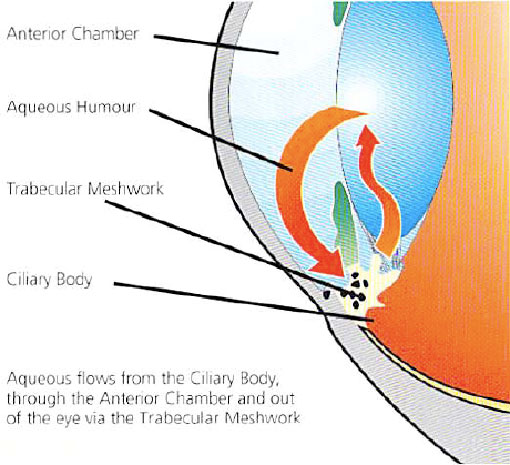
This elevated pressure, in combination with the status of your optic nerve, genetic predisposition, age, and other risk factors, determine the likelihood and rate of development of glaucoma. Primary Open Angle Glaucoma (POAG) is the most common form of glaucoma in Australia and refers to the trabecular meshwork of the eye becoming less efficient at draining aqueous fluid. This can be associated with high or normal intraocular pressures because glaucoma is a type of optic neuropathy—an optic nerve disease. Glaucoma can still affect individuals with “normal” intraocular pressures because the pressure is too high for that particular individual, given his/her specific susceptibility and risk factors.
Angle closure glaucoma occurs when the drainage angle becomes blocked by the peripheral iris (coloured part of the eye). It is more common in persons of Asian decent and those who are long-sighted. As a consequence, no aqueous is able to exit the eye and the intraocular pressure rises.
If angle closure occurs suddenly this is referred to as an acute angle closure attack. This is an ophthalmic emergency and requires urgent treatment to prevent blindness. When the vitreous rubs or pulls on the retina, it creates a sensation of flashing lights.
Booking an appointment
You will require a valid referral to claim your consultation fee and associated investigations from Medicare. Referrals from your GP or Optometrist are valid for 12 months, however specialist referrals are only valid for 3 months.
If you require any specific information regarding your eye problem, for example cataract or glaucoma consultations, we ask you kindly ring your desired practice for fees and further information.
Urgent Appointments
If you have any urgent query or problem, we request that patients or referrers ring the practice directly and speak with a staff member. We will always do our best to accommodate for urgent referrals, or direct you in the best possible manner.
How to reach us?
Dr Brian Chua's primary consulting locations are St Vincent's Clinic and Gordon Eye Surgery.
Please ring us if you require any further information or wish to book an appointment.
St Vincent's Clinic Ophthalmology
Level 10 Suite 1006
438 Victoria Street
Darlinghurst NSW 2010
Ph: 02 8382 6030
Fax: 02 8382 6031
Email: eyedocs1006@stvincents.com.au
Gordon Eye Surgery
2/741 Pacific Highway
Gordon NSW 2072
Ph: 02 9418 1488
Fax: 02 9418 4392
Email: info@gordoneye.com.au
St Vincent's Clinic Ophthalmology
Address: Level 10 Suite 1006
438 Victoria Street Darlinghurst NSW 2010
Tel: 8382 6030
Gordon Eye Surgery
Address: 2/741 Pacific Highway Gordon NSW 2072
Tel: 9418 1488
Lane Cove Eye Surgery
Address: 304/71 Longueville Rd, Lane Cove NSW 2066
Tel: 8377 7600