Diabetic Retinopathy
Diagnosis
A diagnosis can only be made by a full examination by your ophthalmologist. An examination will include dilation of your pupils and may also include an OCT and fluorescein angiography in order to determine the progression of the condition.
An OCT is a cross sectional scan and can detect fluid at the macula. An angiogram involves the injection of dye into the hand or arm. The passage of the dye through the blood vessels supplying the retina can then be observed and photographed for reference.
It can easily be detected during a routine eye check and treatable with laser surgery in the early stages. However it is the leading cause of new blindness in adults.
What Is Diabetic Retinopathy?
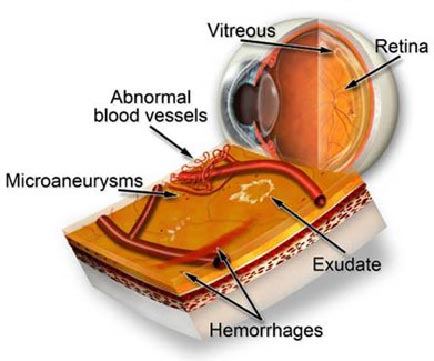
Diabetic retinopathy is an eye condition associated with diabetes. It is caused by the deterioration of the blood vessels which nourish the retina at the back of the eye. As these blood vessels weaken, they may leak fluid or blood, damaging the delicate retina.
Severe visual loss – including total blindness – can result if treatment is not initiated.
Who Is At Risk?
- 6 out of 10 people who have had diabetes for >15 years show symptoms of retinal damage
- Poorly managed diabetes
- High blood sugar levels Gestational diabetes (pregnancy)
Treatment
The most effective way to deal with diabetic retinopathy is prevention. Early diagnosis and correct management of diabetes is essential. Once diagnosed, regular check ups with your ophthalmologist are vital as early treatment improves the chances of preserving vision.
Once it has been determined that background diabetic retinopathy has developed, your doctor may advise laser treatment. Laser treatment is used to seal leaking blood vessels. This is to preserve remaining sight rather than to restore lost vision. It may also be necessary to laser the macula if the swelling does not resolve.
If the macula is involved then injections into the eye of a corticosteroid (triamcinolone) may help to reduce the swelling and inflammation and improve vision. Other drugs may also be given as an injection into the eye and work by causing the new blood vessels to regress.
If proliferative retinopathy has developed, then the doctor may use a laser technique called pan-retinal photocoagulation, which is a type of scatter treatment across the peripheral retina. This helps to minimise the growth of new vessels as well as causing existing abnormal vessels to regress. The laser treatment primarily works to maintain central and colour vision although some peripheral and night vision may be affected. This type of treatment is usually spread over a number of sessions, due to the large amount of retina being treated.
If extensive proliferative retinopathy has developed then a vitrectomy – surgical removal of the vitreous – may be needed. This will remove longstanding blood and scar tissue from inside the eye and maximise the remaining vision.
If this surgery is needed, your doctor will discuss this in more detail with you. If you are diabetic, it is essential that you have a check with your ophthalmologist regularly. Remember that treatment for diabetic retinopathy works to maintain your vision at its current level, so early detection is vital.
Types Of Diabetic Retinopathy
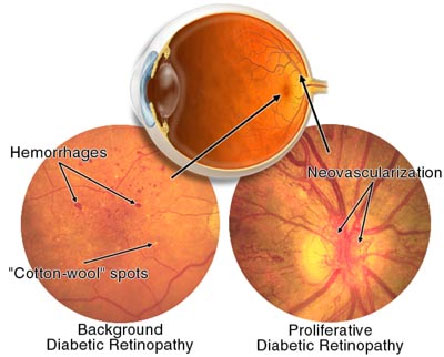
1. Background Retinopathy (Non-proliferative)
This is the most common cause of vision impairment in people with diabetes. It occurs when the blood vessels weaken and leak a clear fluid called serum (or fat) into the surrounding retina. The fluid causes the retina to swell and central vision becomes blurred when the macula (area of sharp vision) is affected. The serum is reabsorbed by the vessels and so blurring lasts a few days at a time. However, if the leakage occurs faster than the serum can be reabsorbed, then the blurring will continue.
The fat deposits are called exudates and are reabsorbed more slowly than the serum. The blood vessels can also bleed into the retina, but vision is not usually affected because the haemorrhages are very small and do not occur within the central macula.
If the central vision is not affected, there may be no symptoms at all. There is no pain or outward symptoms such as bloodshot eyes, irritation or discharge.
Visual symptoms include blurred or distorted vision, problems with reading, watching television and recognising faces, difficulty with glare and night vision.
2. Proliferative Retinopathy
This occurs when new blood vessels grow or “proliferate” over the inner surface of the retina and may even grow out into the vitreous, the clear jelly-like substance inside the eye.
These new vessels, which grow to replace blocked vessels, are weak and bleed easily into the vitreous, causing the vision to become cloudy. Depending on the amount of bleeding, the cloudiness can dissipate within a few days to a few months.
If the bleeding occurs frequently, scar tissue may form between the retina and the vitreous. This may then contract, pulling the retina away from the back of the eye. This is a detached retina and treatment needs to be prompt to prevent complete loss of vision in that eye.
Booking an appointment
You will require a valid referral to claim your consultation fee and associated investigations from Medicare. Referrals from your GP or Optometrist are valid for 12 months, however specialist referrals are only valid for 3 months.
If you require any specific information regarding your eye problem, for example cataract or glaucoma consultations, we ask you kindly ring your desired practice for fees and further information.
Urgent Appointments
If you have any urgent query or problem, we request that patients or referrers ring the practice directly and speak with a staff member. We will always do our best to accommodate for urgent referrals, or direct you in the best possible manner.
How to reach us?
Dr Brian Chua's primary consulting locations are St Vincent's Clinic and Gordon Eye Surgery.
Please ring us if you require any further information or wish to book an appointment.
St Vincent's Clinic Ophthalmology
Level 10 Suite 1006
438 Victoria Street
Darlinghurst NSW 2010
Ph: 02 8382 6030
Fax: 02 8382 6031
Email: eyedocs1006@stvincents.com.au
Gordon Eye Surgery
2/741 Pacific Highway
Gordon NSW 2072
Ph: 02 9418 1488
Fax: 02 9418 4392
Email: info@gordoneye.com.au
St Vincent's Clinic Ophthalmology
Address: Level 10 Suite 1006
438 Victoria Street Darlinghurst NSW 2010
Tel: 8382 6030
Gordon Eye Surgery
Address: 2/741 Pacific Highway Gordon NSW 2072
Tel: 9418 1488
Lane Cove Eye Surgery
Address: 304/71 Longueville Rd, Lane Cove NSW 2066
Tel: 8377 7600