Age-Related Macular Degeneration
What Is Age Related Macular Degeneration?
Age related macular degeneration (AMD) is the most common cause of visual loss in people over 65 years of age. It causes loss of reading or fine vision. However, this disease rarely causes total blindness. and can save enough side vision to ensure independence is maintained.
Risk factors
As the name suggests, age is the major risk factor in AMD. There is also a genetic factor in that it tends to run in families. The major preventable risk factor is smoking.
Diet may also play a part. The most sensible policy is to maintain a well balanced diet, including plenty of fresh fruit and dark green leafy vegetables, nuts and oily fish (salmon, sardines and tuna). This will also help to limit the effects of high blood pressure and cardiovascular disease.
Macuvision and Luteinvision
Developed as a result of international trials, Macu-vision and Lutein-vision are mineral supplements shown to slow down the progression of established AMD.
Treatment
Laser Treatment
Laser treatment is possible in some forms of wet AMD. It aims to preserve as much peripheral retina as possible and prevent severe visual loss by stopping new blood vessels growing. If the new blood vessel can be detected and treated at an early stage, this can significantly increase your chance of avoiding severe visual loss.
Lucentis, Eylea & Avastin Injections
The most recent and most successful treatment for wet AMD has been the use of Lucentis, Eylea and Avastin which are anti-VEGF compounds. VEGF (vascular endothelial growth factor) controls the growth of blood vessels in the body. The anti-VEGF substances act to inhibit the growth of blood vessels and have been found to have a beneficial effect in wet AMD by ‘turning off’ the abnormal blood vessels.
Lucentis and Eylea are given as an injection into the eye, under local anaesthetic, using a fine gauge needle. Initially 3 injections are needed at monthly intervals and then continues, according to clinical progress. The injections, done in the rooms are under sterile conditions, are relatively painless—some people will have eye irritation and intermittent floaters.
With monthly injections, not only is it possible to stop visual loss, but in many cases improve vision. Monthly injections may be required indefinitely, however, the aim being to minimize the number and frequency of injections required by careful monitoring of each patient’s macular thickness by OCT and visual acuity. Newer anti VEGF agents with longer action are also being evaluated, the ideal would be say a once yearly depot injection.
Close follow-up and prompt re-treatment is essential in order to prevent severe visual loss.
If you have been diagnosed with AMD, please check your vision with your Amsler chart regularly. Notify us immediately if you notice
any change in your vision.
How The Eye Works
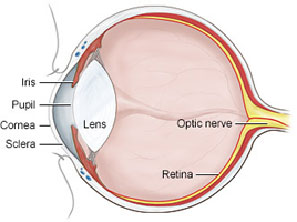
The eye is like a camera. At the front of the eye, the pupil, cornea, and the lens focus the image.
The retina, a light sensitive layer, which lines the back of the eye, receives the image. The image is then sent via the optic nerve to our brain. This is why
glasses do not help us if our poor vision is caused by damage to the retina. Glasses only help the front of the eye to focus the image more clearly.
The Retina
Your retina works like the film in a camera. It must be healthy to work properly. It cannot take a good picture if it is damaged.
The peripheral retina provides us with our side vision. This enables us to navigate, see landscapes and general shapes. In order to see fine detail, we must use the centre of our retina, the macula.
The Macula
The macula is the central area of retina that allows us to see any fine detail. It gives us our reading vision and our ability to recognize faces, watch TV, drive a car or sew etc. The very centre of the macula is called the fovea. The macula is damaged by ageing processes. In the early stages, it shows up as dark dots (pigment clumps) and yellow blobs (drusen).
There are two end stages of macular degeneration that are associated with loss of vision. These are called: Dry (atrophic) or Wet (exudative).
Dry or Atrophic AMD
Patches of retina disappear around the centre of the macula. This is called geographic atrophy and is the most common form of AMD. It is untreatable and eventually involves the fovea, causing slow, progressive loss of reading vision.
Wet or Exudative AMD
This occurs when the barrier which separates the retina from the choroid (the vascular layer beneath the retina) breaks down.
Blood vessels grow from the choroid into the retina. The retina provides ideal conditions for the new blood vessels to grow rapidly. New blood vessels are fragile. They bleed, leak fluid and form a mound of scar tissue. Over time, these blood vessels may continue to grow and destroy more vision. Visual loss may be rapid and severe.
New blood vessels can be seen with special photographs called angiograms and a crosssectional image scan called an OCT.
Angiograms involve a fluorescent vegetable based yellow dye injected into your arm whilst your eye is photographed as the dye passes through the blood vessels in your eye, outlining any abnormalities or leaks.
Sometimes another dye test may be required using an ICG. This shows the blood vessels in the choroid. OCT imaging allows the layers of the retina to be viewed and clearly delineates new blood vessels, drusen and atrophic scarring.
Booking an appointment
You will require a valid referral to claim your consultation fee and associated investigations from Medicare. Referrals from your GP or Optometrist are valid for 12 months, however specialist referrals are only valid for 3 months.
If you require any specific information regarding your eye problem, for example cataract or glaucoma consultations, we ask you kindly ring your desired practice for fees and further information.
Urgent Appointments
If you have any urgent query or problem, we request that patients or referrers ring the practice directly and speak with a staff member. We will always do our best to accommodate for urgent referrals, or direct you in the best possible manner.
How to reach us?
Dr Brian Chua's primary consulting locations are St Vincent's Clinic and Gordon Eye Surgery.
Please ring us if you require any further information or wish to book an appointment.
St Vincent's Clinic Ophthalmology
Level 10 Suite 1006
438 Victoria Street
Darlinghurst NSW 2010
Ph: 02 8382 6030
Fax: 02 8382 6031
Email: eyedocs1006@stvincents.com.au
Gordon Eye Surgery
2/741 Pacific Highway
Gordon NSW 2072
Ph: 02 9418 1488
Fax: 02 9418 4392
Email: info@gordoneye.com.au